COVID-19 Disproportionately Hurts the Elderly, Obese, and Poor
My recent work on COVID-19 has revealed four main conclusions. First, COVID-19 attacks those over 54; only 1,019 people under 25 died. Second, there are four common COVID-19 related death comorbidities. Three, those who struggle with obesity are highly vulnerable, and government policy has not helped. Fourth, the response by governments has pushed 150 million people into poverty. All the data I reveal in this research comes from traditional sources and can be accessed through hyperlinks.
COVID-19 attacks those over 54; only 1,019 people under 25 died
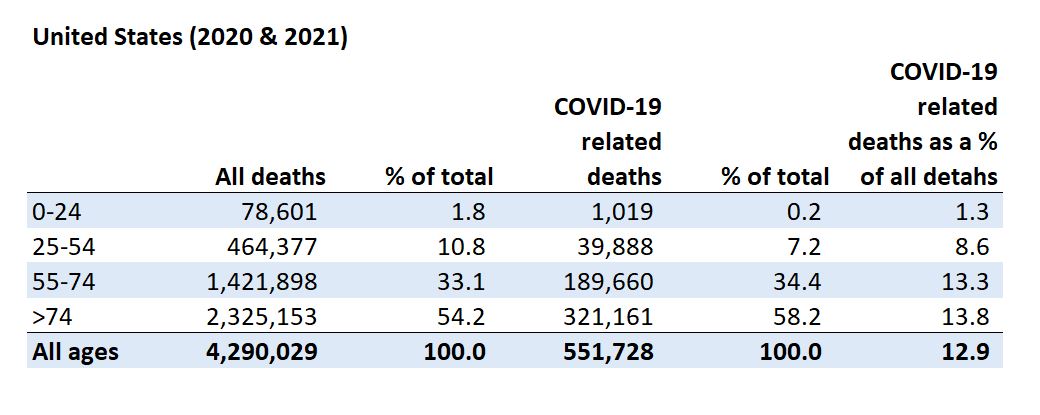
We start with good news; according to recently updated data, only 1,019 people under 25 died of COVID-19 since the beginning of 2020. This group accounted for about 0.2% of all COVID-19 deaths in the US. Another 39,888 died within the age range of 25 to 54. This means that about 93% of all COVID-19 deaths were over 55; 58% were over 74 years old. Again, the good news is that COVID-19 is not killing young people.
Four common COVID-19 related death comorbidities
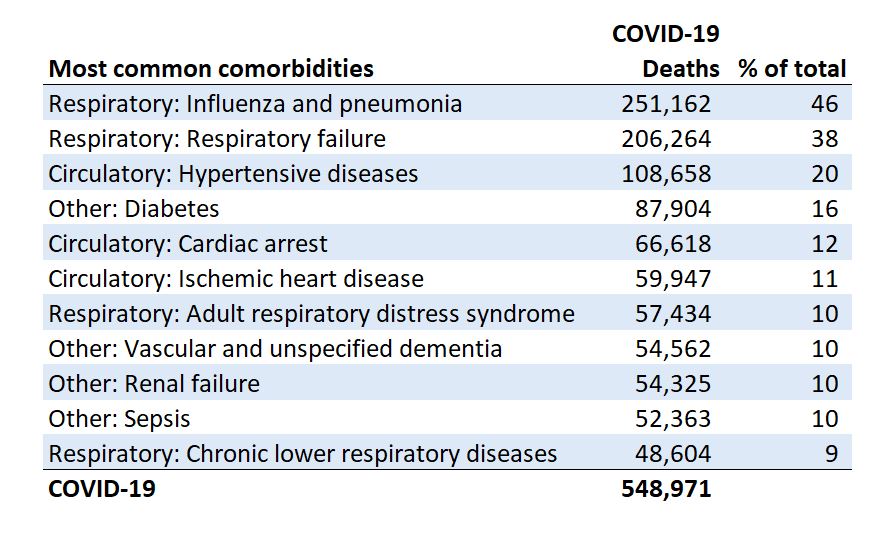
According to the Oxford dictionary, comorbidity is “the simultaneous presence of two or more diseases or medical conditions in a patient.” Death certificate data provided by the CDC reveal the causes of death in addition to SARS-CoV-2. Since people could have more than one comorbidity, the percentages below do not add up to 100%.
In addition to COVID-19, respiratory diseases, influenza, and pneumonia were noted on COVID-19 related death certificates 46% of the time. The next most common was a respiratory failure which was mentioned 38% of the time. The next most significant comorbidity was hypertensive diseases, which are within the circulatory diseases group. Hypertension appeared on death certificates 20% of the time. The fourth most common comorbidity was diabetes, which occurred 16% of the time.
Another research paper published in February 2021 showed that hypertension, obesity, and diabetes were the most prevalent comorbidities in COVID-19 patients. They also highlighted that cancer, chronic kidney diseases, diabetes, and hypertension were independently associated with mortality in COVID-19 patients. Finally, they found that chronic kidney disease was the most prominent comorbidity leading to death.
The CDC has been updating its guidance related to comorbidities, which currently shows that the most common comorbidities were hypertension at 47%, hyperlipidemia (high levels of lipids-fats, cholesterol, or triglycerides-circulating in the blood) at 29%, diabetes at 28%, and chronic pulmonary disease 16%.
Obese are highly vulnerable and government policy has not helped
What is obesity?
According to Wikipedia, “obesity is a medical condition in which excess body fat has accumulated to the extent that it may have a negative effect on health. It is correlated with various diseases and conditions, particularly cardiovascular diseases, type 2 diabetes, obstructive sleep apnea, certain types of cancer, and osteoarthritis. There have also been links found between obesity and depression. Research shows that maintaining weight loss after dieting over the long term proves to be rare.”
“Diet quality can be improved by reducing the consumption of energy-dense foods, such as those high in fat or sugars, and by increasing the intake of dietary fiber. However, studies have found an inverse relationship between energy density and energy cost of foods in developed nations. Low-income populations are more likely to live in neighborhoods that are considered “food deserts” or “food swamps” where nutritional groceries are less available.”
“Obesity is a leading preventable cause of death worldwide, with increasing rates in adults and children. In 2015, 600 million adults (12%) and 100 million children were obese in 195 countries. Authorities view it as one of the most serious public health problems of the 21st century.”
Obesity afflicts more than 20% of adults in Americans
Guidelines related to obesity are issued by the CDC, which gives these definitions:
- Overweight – Body mass index (BMI) > 25 kg/m2 but < 30 kg/m2
- Obesity – BMI ≥30 kg/m2 but < 40 kg/m2
- Severe obesity – BMI of ≥40 kg/m2
A recent CDC study in America showed that “All states and territories had more than 20% of adults with obesity.”
Education level is a significant determinate of the risk of obesity
Under the CDC, the US Behavioral Risk Factor Surveillance System conducts more than 400,000 telephone surveys per year across all 50 states and concluded that about 34% of those who had not graduated from college self-reported as obese, which was much lower at 25% for college grads.
Guidelines about how Americans should refer to obesity
The CDC refers to notes on language and images to use and not use concerning obesity. They recommend the following:
- Say, “adults with obesity” or “20% of children ages 12-19 have obesity.”
- Don’t say “obese adults” nor “20% of children are obese.”
These guidelines originate from the Guidelines for Media Portrayals of Individuals Affected by Obesity. What follows comes from this report, “Consider carefully whether terminology and language used to describe body weight could be offensive to persons with obesity and how the intended audience will interpret this language. Avoid using potentially pejorative adjectives or adverbs when describing people who are affected by excess weight or obesity and language that implies moral judgments or character flaws of this population.”
Early on, governments knew the relationship between COVID-19 death and obesity
In July 2020, the UK govt issued a press release that highlighted a research study that found that for people with a BMI of 35 to 40, the risk of death from COVID-19 increases by 40%, and those with a BMI over 40 by 90%, compared to those not living with obesity.
Other data found that in intensive care units, 7.9% of critically ill patients with COVID-19 had a BMI over 40 compared with 2.9% of the general population.
Almost two-thirds (63%) of adults in England are overweight or obese, with people aged 55 to 74, those living in deprived areas, and certain black, Asian, and minority ethnic groups more severely affected.
In the US in August 2020, a meta-study of peer-reviewed papers found that people with obesity who contracted SARS-CoV-2 were 113% more likely than people of healthy weight to land in the hospital, 74% more likely to be admitted to an ICU, and 48% more likely to die.
Italy was an early warning about the deadliness of COVID-19
Wikipedia reveals that COVID-19 spread to Italy on 31 January 2020, with the first deaths on 22 February. By the beginning of March, the virus had spread to all regions of Italy.
Economic shut down meant less exercise and more energy-dense (read: fattening) foods
One study reviewed the impact of the breakdown of supply chains. This breakdown limited access to fresh foods, leading to an abundance of processed and ultra-processed foods, which are energy dense and contain saturated fat, sodium, and sugar.
Ultra-processed foods have previously been found to be directly linked to obesity and adverse health outcomes. Due to the low cost of ultra-processed food, this supply chain breakdown hit the population’s lower-income segments hardest.
Lockdowns reduced the walking and exercise time of adults, causing a rise in obesity. Reduced energy expenditures and increased ultra-processed foods have likely contributed to significant weight gain.
To make matters worse, health professionals previously know that individuals with obesity are likely to face reductions in vaccines’ effectiveness through mechanisms similar to those responsible for greater primary infection risk.
Government shelter-in-place orders cost about 7 kg of permanent weight gain
A recent study showed that the cost of complying with the US government’s shelter-in-place (SIP) orders was a steady weight gain of 0.27 kg (0.6 lbs) every ten days irrespective of geographic location or comorbidities of the subjects studied. This translates into about 0.7 kg (1.5 lbs) of weight gain every month, which means that this policy alone could have caused the average American to gain about 7 kg (15 lbs). Additional research shows that this weight gain is likely to be permanent.
Obesity is deadly
One study showed that before the pandemic, around 2.8 million people worldwide died each year because of being overweight, from conditions that stem from it, including heart disease, stroke, and diabetes.
COVID-19 deaths per million were 10x higher in above-average obesity countries
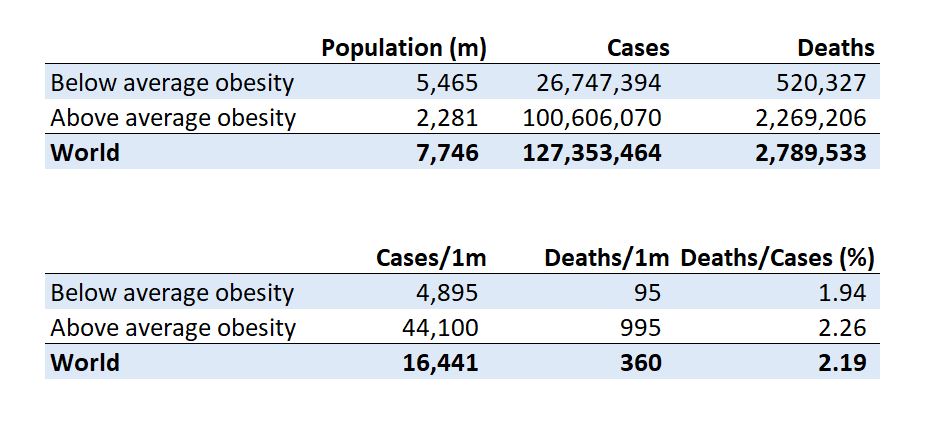
We accessed World Health Organization’s data on obesity and COVID-19 disease data from Wikipedia to rank 171 countries on these two measures. We split the list of countries in half; of the 85 countries with below-average obesity rates, the lowest were: Vietnam, Bangladesh, Cambodia, India, Nepal, and Japan. Of the 86 countries with the highest obesity, the worst were: United States, Jordan, Saudi Arabia, Turkey, and Egypt.
The table below shows that above-average countries had 9x more cases per 1,000,000 people and 10x more deaths per 1,000,000 people. The death rate for those infected was only slightly higher, possibly because those who got COVID-19 in the below-average obesity countries were the rare obese citizens.
A widely available study shows a clear link between obesity and death from COVID-19
Don’t take my word for it; a recent study from the World Obesity Federation also found that COVID-19 death rates are ten times higher in countries where more than half of the adult population is classified as overweight. “Of the 2.5 million COVID-19 deaths reported by the end of February 2021, 2.2 million were in countries where over half the population is classified as overweight—defined as a body mass index above 25.”
The report found linear correlations between a country’s COVID-19 mortality and the proportion of overweight adults. They also found that not a single nation with less than 40% of the population overweight had high death rates, and no country with a high death rate had less than 50% of their population overweight.
The report highlighted that 68% of the US population was overweight compared to only 18% in Vietnam.
A November 2020 paper referenced 22 previously published peer-reviewed articles linking obesity and its impact on COVID-19 outcomes. It concluded that obesity had a substantial effect on risk related to COVID-19. The paper recommended that obese patients receive more aggressive preventative measures.
Why are the obese so vulnerable to COVID-19?
One recent study proposed the following seven potential reasons why COVID-19 more hard-hit the obese
- Obesity-associated inflammation and its impact on SARS-CoV-2 infection
- Cellular immune function is impaired in obesity
- Excess fat deposition disrupts lymphoid tissue architecture and integrity
- Insulin resistance negatively impact immune function
- Leptin resistance in obesity impairs immune functioning
- Altered ACE2 expression in obese subjects may affect COVID-19 disease severity
- Role of coagulopathy /thrombosis in SARS-CoV-2 pathogenesis
Response by governments has pushed 150 million people into poverty
Governments worldwide have shut down their economies in response to COVID-19, and the health and economic costs have been devastating to hundreds of millions. Billionaires get richer, politicians continue to collect their regular pay, and the middle and upper-middle-class knowledge workers have fared relatively well. Some in these groups may have actually benefited from the government’s low-interest policy and support for the stock and bond markets.
Nearly 150 million people pushed into poverty
In Oct 2020, the World Bank’s biennial Poverty and Shared Prosperity Report revealed that the COVID-19 related government economic shutdowns were expected to push about 100 million people into extreme poverty (less than US$1.9 per day) in 2020, and another 50 million people could be added on to that in 2021.
67 million in India fell to “Poor” status, while 28 million in China fell to “Low income”
A Pew Research Center study found that because of the COVID-19 economic shutdown, about 67 million people in India fell from middle and low income to the status of “Poor,” which means they now live on US$2 or less a day. They estimate that in China, 28 million people fell from upper-middle and middle income to low income, meaning they now live on US$2 to US$10 per day.
An additional 142 million children now live in poor households
A UNICEF and Save the Children joint report shows that a pessimistic estimate is that the COVID-19 economic shutdowns caused an additional 142 million children to live in poor households.
11% of US adults say sometimes, or often they don’t have enough to eat
An early March 2021 Household Pulse Survey revealed that in America, about 22 million adults, 11% of all adults, reported that their household “sometimes or often” didn’t have enough to eat in the last seven days. The answer to this question in 2019 was about 3.4% of adults, meaning the problem has gotten nearly four times worse.
DISCLAIMER: This content is for information purposes only. It is not intended to be investment advice. Readers should not consider statements made by the author(s) as formal recommendations and should consult their financial advisor before making any investment decisions. While the information provided is believed to be accurate, it may include errors or inaccuracies. The author(s) cannot be held liable for any actions taken as a result of reading this article.